Abstract
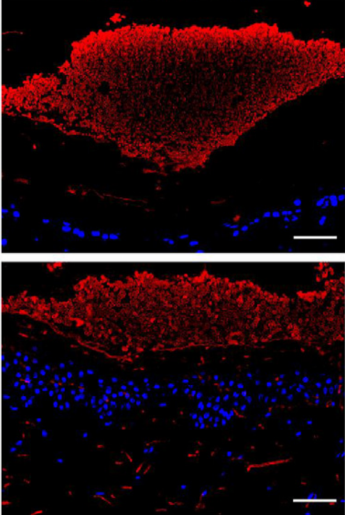
The World Health Organization (WHO) declared certain fungal pathogens as global health threats for the next decade. Candida auris (C. auris) is a newly emerging skin-tropic multidrug-resistant fungal pathogen that can cause life-threatening infections of high mortality in hospitals and healthcare settings. Here, we address an unmet need and present novel native ex vivo skin models, thus extending previous C. auris-host interaction studies. We exploit histology and immunofluorescence analysis of ex vivo skin biopsies of human adult and fetal, as well as mouse origin infected with C. auris via distinct routes. We demonstrate that an intact skin barrier efficiently protects from C. auris penetration and invasion. Although C. auris readily grows on native human skin, it can reach deeper layers only upon physical disruption of the barrier by needling or through otherwise damaged skin. By contrast, a barrier disruption is not necessary for C. auris penetration of native mouse skin. Importantly, we show that C. auris undergoes morphogenetic changes upon skin penetration, as it acquires pseudohyphal growth phenotypes in deeper human and mouse dermis. Taken together, this new human and mouse skin model toolset yields new insights into C. auris colonization, adhesion, growth and invasion properties of native versus damaged human skin. The results form a crucial basis for future studies on skin immune defense to colonizing pathogens, and offer new options for testing the action and efficacy of topical antimicrobial compound formulations.